
ASE SUMMARYA
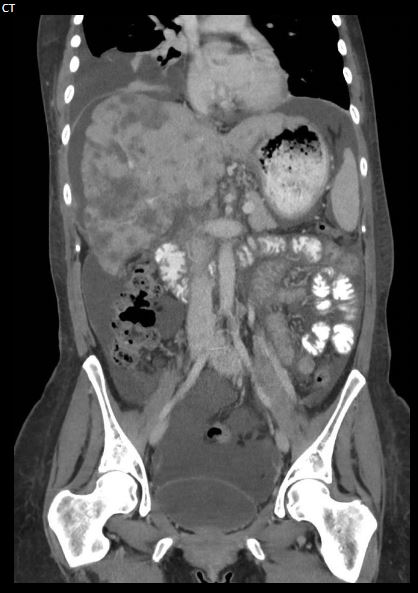
patient with a history of metastatic breast cancer with liver involvement status post-chemotherapy treatment presented for an ultrasound evaluation with a new complaint of abdominal distension.IMAGING FINDINGSUltrasound and CT scans of the abdomen demonstrated a markedly nodular liver contour and heterogeneous echotexture with innumerable masses throughout the hepatic parenchyma. A moderate volume of ascites was seen in the abdomen. Findings are compatible with pseudocirrhosis in the setting of treated metastatic disease.
FINAL DIAGNOSIS: Pseudocirrhosis

Although pseudocirrhosis has been most frequently described in post-chemotherapy patients with liver metastases from breast cancer, the condition has also been reported in association with other malignancies. The underlying physiology of pseudocirrhosis is still unclear. However, according to multiple theories, chemotherapy-induced liver injury is the critical component initiating the development of the condition. It is theorized that chemotherapy causes hepatocyte injury, leading to ischemic atrophy and regenerative nodular hyperplasia in regions with favorable blood flow. These regenerative nodules and other features like capsular retractionresulting from hepatic injury cause the imaging appearance that mimics liver cirrhosis.
Patients affected by pseudocirrhosis may be asymptomatic. In such cases, the condition is identified incidentally on surveillance imaging. Most commonly, however, pseudocirrhosis is associated with complications of portal hypertension, and abdominal distension with ascites is the typical initial presentation

The imaging features of pseudocirrhosis are similar to true cirrhosis. These features include nodularity of the liver contour, diffuse parenchymal heterogeneity, capsular retraction, liver atrophy, caudate lobe enlargement, and portal hypertension signs such as ascites splenomegaly and varices. Compared with true liver cirrhosis, pseudocirrhosis progresses rapidly. For that reason, it is not difficult to detect serial changes in the liver morphology on surveillance imaging. At first, the liver shows a smooth hepatic surface with metastases which may focally bulge out. However, with time, capsular retraction and parenchymal atrophy become more prominent, exaggerating the appearance of metastases and regenerative nodules.
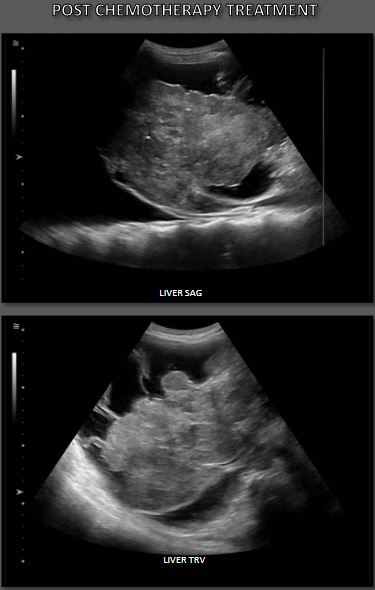
Pseudocirrhosis is a devastating complication of metastatic breast cancer. The rapid onset and progression of pseudocirrhosis to liver failure tremendously affect the treatment outcome and can be highly lethal. Pseudocirrhosis negatively impacts the ability of patients to tolerate further chemotherapy for breast cancer, impacting the management strategy and shortening their survival rate. Once the diagnosis of pseudocirrhosis is made, some patients require a change in chemotherapy drugs, whereas some have to permanently discontinue chemotherapy and transition to supportive care only.93-96LIVER SAGA markedly nodular liver contour with capsular retraction and heterogeneous parenchymal echotexture with innumerable masses represents pseudocirrhosis in the setting of treated metastatic disease.CTTRV84
'on the wavelength > abdomen' 카테고리의 다른 글
| Duplication of gallbladder/cholecystectomy/ (0) | 2023.04.15 |
|---|---|
| biliary stone /Choledocholithiasis/CBD stone /sono (0) | 2023.04.15 |
| Focal nodular hyperplasia/FNH liver/central scar (0) | 2023.04.14 |
| Hepatitis/acute hepatitis (0) | 2023.04.14 |
| polycystic liver disease (PLD) (0) | 2023.04.14 |




댓글